From Wikipedia, the free encyclopedia
| Benzodiazepines |
|---|
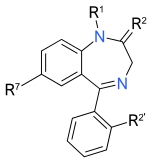 |
| The core structure of benzodiazepines. “R” labels denote common locations of benzodiazepines their unique properties. |
| Benzodiazepine |
| List of benzodiazepines |
| Benzodiazepine overdose |
| Benzodiazepine dependence |
| Benzodiazepine drug misuse |
| Benzodiazepine withdrawal syndrome |
| Long-term effects of benzodiazepines |
A benzodiazepine (pronounced /ˌbɛnzɵdaɪˈæzɨpiːn/, sometimes abbreviated to “benzo“) is a psychoactive drug whose core chemical structure is the fusion of a benzene ring and a diazepine ring. The first benzodiazepine, chlordiazepoxide (Librium), was discovered accidentally by Leo Sternbach in 1955, and made available in 1960 by Hoffmann–La Roche, which has also marketed diazepam (Valium) since 1963.[1]
Benzodiazepines enhance the effect of the neurotransmitter gamma-aminobutyric acid, which results in sedative, hypnotic (sleep-inducing), anxiolytic (anti-anxiety), anticonvulsant, muscle relaxant and amnesic action.[2] These properties make benzodiazepines useful in treating anxiety, insomnia, agitation, seizures, muscle spasms,
Benzodiazepines are generally safe and effective in the short term, although cognitive impairments and
There is controversy concerning the safety of benzodiazepines in pregnancy. While they are not major
Contents[hide] |
[edit] History

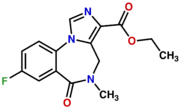
The molecular structure of chlordiazepoxide, the first benzodiazepine. It was marketed by Hoffmann–La Roche from 1960 branded as Librium.
The first benzodiazepine, chlordiazepoxide (Librium), was synthesized in 1955 by Leo Sternbach while working at Hoffmann–La Roche on the development of tranquilizers. The pharmacological properties of the compounds prepared initially were disappointing, and Sternbach abandoned the project. Two years later, in April 1957, co-worker Earl Reeder noticed a “nicely crystalline” compound left over from the discontinued project while spring cleaning in the lab. This compound, later named chlordiazepoxide, had not been tested in 1955 because of Sternbach’s focus on other issues. Expecting the pharmacology results to be negative and hoping to publish the chemistry-related findings, researchers submitted it for a standard battery of animal tests. Unexpectedly, the compound showed very strong sedative, anticonvulsant and muscle relaxant effects. These impressive clinical findings led to its speedy introduction throughout the world in 1960 under the brand name Librium.[16][17] Following chlordiazepoxide, diazepam was marketed by Hoffmann–La Roche under the brand name Valium in 1963, and for a while the two were the most commercially successful drugs. The introduction of benzodiazepines led to a decrease in the prescription of barbiturates, and by the 1970s they had largely replaced the older drugs for sedative and hypnotic uses.[1]
The new group of drugs was initially greeted with optimism by the medical profession, but gradually concerns arose; in particular, the risk of dependence became evident in the 1980s. Benzodiazepines have a unique history in that they were responsible for the largest ever
Although antidepressants with anxiolytic properties have been introduced, and there is increasing awareness of the adverse effects of benzodiazepines, prescriptions for short term anxiety relief drugs have not significantly dropped.[6] For treatment of insomnia, benzodiazepines are now less popular than nonbenzodiazepines, which include zolpidem, zaleplon, eszopiclone, and ramelteon.[20] Nonbenzodiazepines are molecularly distinct, but nonetheless, they work on benzodiazepine receptors.[21]
[edit] Therapeutic uses
Benzodiazepines possess sedative, hypnotic, anxiolytic, anticonvulsant, muscle relaxant and amnesic actions,[2][3] which are useful in a variety of indications such as alcohol dependence,
[edit] Panic disorder
Because of their effectiveness, tolerability and rapid onset of anxiolytic action, benzodiazepines are frequently used for the treatment of anxiety associated with panic disorder.[27] There is disagreement among expert bodies regarding the long-term use of benzodiazepines for panic disorder. The views range from benzodiazepines being not effective long-term,[28] that they should be reserved for treatment resistant cases[29] or that they are as effective in the long-term as the main alternative agents,
The American Psychiatric Association (APA) guidelines[30] note that benzodiazepines are generally well tolerated and their use as an initial treatment for panic disorder is strongly supported by numerous controlled trials. APA states that there is insufficient evidence to recommend any of the established panic disorder treatments over another. The choice of treatment between benzodiazepines,
Guidelines issued by the UK-based National Institute for Health and Clinical Excellence (NICE) do not recommend use of benzodiazepines beyond two to four weeks, as tolerance and physical dependence develop rapidly, with withdrawal symptoms including
Benzodiazepines are usually administered orally; however, very occasionally lorazepam or diazepam may be given intravenously for the treatment of
[edit] Generalized anxiety disorder
Benzodiazepines have robust efficacy in the short-term management of generalized anxiety disorder (GAD), but were not shown to be effective in producing long-term improvement overall.[33] According to National Institute for Health and Clinical Excellence (NICE), benzodiazepines can be used in the immediate management of GAD, if necessary. However, they should not usually be given for longer than 2-4 weeks. The only medications NICE recommends for the longer term management of GAD are antidepressants.[34]
Similarly, Canadian Psychiatric Association (CPA) recommends benzodiazepines alprazolam, bromazepam, lorazepam, and diazepam only as a second-line choice, if the treatment with two different antidepressants was unsuccessful. Although they are second-line agents, benzodiazepines can be used for a limited time to relieve severe anxiety and agitation. CPA guidelines note that after 4-6 weeks the effect of benzodiazepines may decrease to the level of placebo, and that benzodiazepines are less effective than antidepressants in alleviating ruminative worry, the core symptom of GAD. However, in some cases a prolonged treatment with benzodiazepines as the add-on to an antidepressant may be justified.[35]
[edit] Insomnia
Benzodiazepines are useful for a short-term treatment of insomnia. They improve the quality of sleep by shortening the time spent in bed before falling asleep, prolonging the sleep time and generally reducing wakefulness. However, their use beyond four weeks is not recommended due to the risk of dependence. Preferably, benzodiazepines are taken intermittently and at the lowest effective dose.[36][37] Other drawbacks of hypnotics, including benzodiazepines, are possible tolerance to their effects,
It is not clear whether the new nonbenzodiazepine hypnotics (Z-drugs) are better than the short-acting benzodiazepines. The efficacy of these two groups of medications is similar.[36][38] According to the US Agency for Healthcare Research and Quality, indirect comparison indicates that side effects from benzodiazepines may be about twice as frequent as from nonbenzodiazepines.[38] This may make the non-benzodiazepines preferable as the first-line long-term treatment of insomnia.[37] However, the UK National Institute for Health and Clinical Excellence did not find any convincing evidence in favor of Z-drugs. NICE review pointed out that short-acting Z-drugs were inappropriately compared in clinical trials with long-acting benzodiazepines. There have been no trials comparing short-acting Z-drugs with appropriate doses of short-acting benzodiazepines. Based on this, NICE recommended choosing the hypnotic based on cost and patient’s preference.[36]
It has been argued that long term use of
[edit] Seizures
Prolonged convulsive
When benzodiazepines were first introduced, they were enthusiastically adopted for treating all forms of epilepsy. However, drowsiness and tolerance become problems with continued use and none are now considered first-line choices for long-term epilepsy therapy.[42] Clobazam is widely used by specialist epilepsy clinics worldwide (but it is not available in the US) and clonazepam is popular in France.[42] In the UK, both clobazam and clonazepam are second-line choices for treating many forms of epilepsy.[43] Clobazam also has a useful role for very short-term seizure prophylaxis and in catamenial epilepsy.[42] Discontinuation after long term use in epilepsy requires additional caution because of the risks of rebound seizures. Therefore, the dose is slowly tapered over a period of up to six months or longer.[41]
[edit] Alcohol withdrawal
Chlordiazepoxide is the most commonly used benzodiazepine for alcohol detoxification,[44] but diazepam may be used as an alternative. Both are used in the detoxification of individuals who are motivated to stop drinking, and are prescribed for a short period of time to reduce to the risks of tolerance and dependence to the benzodiazepine medication itself.[22]:275 The benzodiazepines with a longer half life make detoxification more tolerable, and dangerous alcohol withdrawal effects are less likely to occur. On the other hand, short-acting benzodiazepines may lead to breakthrough seizures, and are therefore not recommended for detoxification in an outpatient setting. Oxazepam and lorazepam are often used in patients at risk of drug accumulation, particularly the elderly and those with cirrhosis, because they are metabolized differently from other benzodiazepines, through conjugation.[45][46]
Benzodiazepines are the preferred choice in the management of alcohol withdrawal syndrome, particularly for the prevention and treatment of the dangerous complication of seizures and in subduing severe delirium.[47] Lorazepam is the only benzodiazepine with predictable intramuscular absorption and it is the most effective in preventing and controlling acute seizures.[48]
[edit] Anxiety
Benzodiazepines are sometimes used in the treatment of acute anxiety as they bring about rapid and marked or moderate relief of symptoms in most individuals[28]; however, they are not recommended beyond 2-4 weeks of use due to risks of tolerance and dependence and a lack of long-term effectiveness. Compared to other pharmacological treatments benzodiazepines are twice as likely to lead to a relapse of the underlying condition upon discontinuation. Psychological therapies and other pharmacological therapies are recommended for the long-term treatment of generalised anxiety disorder. Antidepressants have higher remission rates and are safe and effective in the short and long-term.[28]
[edit] Other indications
Benzodiazepines are often prescribed for a wide range of conditions. Some of the most notable indications are summarised below.
- They can be very useful in intensive care to sedate patients receiving mechanical ventilation, or those in extreme distress. Caution is exercised in this situation due to the occasional occurrence of
respiratory depression; it is recommended that benzodiazepine overdose treatment facilities should be available.[49]
- They are effective as premedication given a couple of hours before surgery to relieve anxiety. They also produce amnesia, which can be useful as patients will not be able to remember any unpleasantness from the procedure.[49] Diazepam or temazepam can be used in patients who are particularly anxious about dental procedures and some ophthalmic procedures like refractive surgery, or for example those with
dental phobia.[49] Midazolam is the most commonly prescribed for this use because of its strong sedative actions and fast recovery time, as well as its water solubility which reduces pain upon injection. Diazepam and lorazepam are sometimes used; lorazepam has particularly marked amnesic properties that may make it more effective when amesia is the desired effect.[22]:693
- Benzodiazepines are well known for their strong muscle-relaxing properties and can be useful in the treatment of muscle spasms,[22]:577–578 although tolerance often develops to their muscle relaxant effects.[8] Baclofen is sometimes used as an alternative to benzodiazepines.[50]
- Benzodiazepines are also used to treat the acute panic caused by
hallucinogen intoxication,[51] Benzodiazepines are also used to calm the acutely agitated individual and can, if required, be given via an intramuscular injection.[52] They can sometimes be effective in the short-term treatment of psychiatric emergencies such as acute psychosis as in schizophrenia or mania, bringing about rapid tranquillization and sedation until the effects of lithium or neuroleptics (antipsychotics) take effect. Lorazepam is most commonly used but clonazepam is sometimes prescribed for acute psychosis or mania;[53][54] their long-term use is not recommended due to risks of dependence.[22]:204
[edit] Side effects
The most common side effects of benzodiazepines are related to their sedating and muscle-relaxing action. They include
[edit] Paradoxical effects
[edit] Cognitive effects
The short-term use of benzodiazepines adversely affects multiple areas of cognition; most notably, it interferes with the formation and consolidation of memories of new material and may induce complete anterograde amnesia.[55] However, researchers hold contrary opinions regarding the effects of long-term administration. One view is that many of the short-term effects continue into the long-term and may even worsen, and are not resolved after quitting benzodiazepines. Another view maintains that cognitive deficits in chronic benzodiazepine users occur only for a short period after the dose, or that the anxiety disorders is the cause of these deficits. While the definitive studies are lacking, the former view recently received support from a meta-analysis of 13 small studies.[64][65] This meta-analysis found that long-term use of benzodiazepines was associated with moderate to large adverse effects on all areas of cognition, with
[edit] Long-term effects
The long-term adverse effects of benzodiazepines include a general deterioration in physical and mental health and tend to increase with time. Not everyone however, experiences problems with long-term use. The adverse effects can include cognitive impairments and affective and behavioural problems. Feelings of turmoil, difficulty in thinking constructively, loss of sex-drive, agoraphobia and social phobia, increasing anxiety and depression, loss of interest in leisure pursuits and interests, an inability to experience or express feelings also occurs.[9][66] Additionally an altered perception of self, environment and relationships may occur.[65]
[edit] Withdrawal syndrome
[edit] Tolerance, dependence and withdrawal

Diazepam 2 mg and 5 mg diazepam tablets, which are commonly used in the treatment of
The main problem of the chronic use of benzodiazepines is the development of tolerance and dependence. Tolerance manifests itself as diminished pharmacological effect and develops relatively quickly to the sedative, hypnotic, anticonvulsant and muscle relaxant actions of benzodiazepines. Tolerance to anti-anxiety effects develops more slowly with little evidence of continued effectiveness beyond four to six months of continued use. Tolerance to the amnesic effects, generally, does not occur.[8][67] However, controversy exists as to tolerance to the anxiolytic effects with some evidence that benzodiazepines retain efficacy[68] and opposing evidence from a systematic review of the literature that tolerance frequently occurs[23][28] and some evidence that anxiety may worsen with long-term use.[8] The question of tolerance to the amnesic effects of benzodiazepines is similarly unclear.[69] Some evidence suggests that partial tolerance does develop, and “the memory impairment is limited to a narrow window within 90 minutes after each dose”.[70]
Discontinuation of benzodiazepines or abrupt reduction of the dose, even after a relatively short course of treatment (three to four weeks), may result in two groups of symptoms—rebound and withdrawal. Rebound symptoms are the return of the symptoms for which the patient was treated but worse than before. Withdrawal symptoms are the new symptoms that occur when the benzodiazepine is stopped. They are the main sign of physical dependence.[70]
[edit] Withdrawal symptoms and management

Chlordiazepoxide 5 mg capsules which are sometimes used as an alternative to diazepam for
The most frequent symptoms of withdrawal from benzodiazepines are insomnia, gastric problems, tremors, agitation, fearfulness and muscle spasms.[70] The less frequent effects are irritability, sweating, depersonalization, derealization, hypersensitivity to stimuli, depression,
Symptoms may also occur during a gradual dosage reduction, but are typically less severe and may persist as part of a protracted withdrawal syndrome for months after cessation of benzodiazepines.[72] Approximately 10% of patients will experience a notable protracted withdrawal syndrome which can persist for many months or in some cases a year or longer. Protracted symptoms tend to resemble those seen during the first couple of months of withdrawal but usually are of a sub acute level of severity. Such symptoms do gradually lessen over time, eventually disappearing altogether.[73]
Benzodiazepines have a reputation with patients and doctors for causing a severe and traumatic withdrawal; however, this is in large part due to the withdrawal process being poorly managed. Over-rapid withdrawal from benzodiazepines increases the severity of the withdrawal syndrome and increases the failure rate. A slow and gradual withdrawal customised to the individual and, if indicated, psychological support is the most effective way of managing the withdrawal. Opinion as to the time needed to complete withdrawal ranges from four weeks to several years. A goal of less than six months has been suggested,[7] but due to factors such as dosage and type of benzodiazepine, reasons for prescription, lifestyle, personality,
Withdrawal from long term benzodiazepines is benefitial for most individuals.[63] Withdrawal of benzodiazepines from long term users generally leads to improved physical and mental health particularly in the elderly; however, some long term users report continued benefit from taking benzodiazepines, but this may be the result of suppression of withdrawal effects.[8][9]
[edit] Contraindications
Because of their muscle relaxant action, benzodiazepines may cause respiratory depression in susceptible individuals. For that reason, they are contraindicated in people with myasthenia gravis, sleep apnea, bronchitis and COPD.[55][77] Caution is required when benzodiazepines are used in people with
[edit] Pregnancy

Benzodiazepines taken during pregnancy have adverse effects on the baby. Abrupt withdrawal in
In the United States, the Food and Drug Administration has categorized benzodiazepines into either category D or X meaning potential for harm in the unborn has been demonstrated.[80]
Exposure to benzodiazepines during pregnancy has been associated with a slightly increased (from 0.06 to 0.07%) risk of cleft palate in newborns, a controversial conclusion as some studies find no association between benzodiazepines and cleft palate. Their use by expectant mothers shortly before the delivery may result in a floppy infant syndrome, with the newborns suffering from hypotonia,
[edit] Elderly

Adverse effects of benzodiazepines are increased in the elderly. Adverse effects on cognition can be mistaken for the effects of old age.[84]
The benefits of benzodiazepines are least and the risks are the greatest in the elderly.[85] The elderly are at an increased risk of
Long-term use of benzodiazepines has been associated with increased risk of cognitive impairment, but its relationship with dementia remains inconclusive.[87] The association of a past history of benzodiazepine use and cognitive decline is unclear, with some studies reporting a lower risk of cognitive decline in former users, some finding no association and some indicating an increased risk of cognitive decline.[88]
Benzodiazepines are sometimes prescribed to treat behavioral symptoms of dementia. However, similarly to antidepressants they have little evidence of effectiveness, although antipsychotics have shown some benefit.[89][90] Cognitive impairing effects of benzodiazepines which occur frequently in the elderly can also worsen dementia.[91]
[edit] Pharmacology
Benzodiazepines share a similar chemical structure and their effects in humans are mainly produced by the
[edit] Chemistry
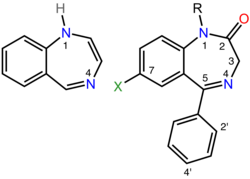
Left: The 1,4-benzodiazepine ring system. Right: 5-phenyl-1H-benzo[e][1,4]diazepin-2(3H)-one forms the skeleton of many of the most common benzodiazepine pharmaceuticals, such as diazepam (7-chloro-1-methyl substituted). |
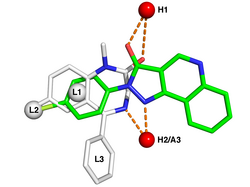
A pharmacophore model of the benzodiazepine binding site on the GABAA receptor.[95] White sticks represent the carbon atoms of the benzodi-azepine diazepam while green represents carbon atoms of the nonbenzodiazepine CGS-9896. Red and blue sticks are oxygen and nitrogen atoms that are present in both structures. The red spheres labeled H1 and H2/A3 are respectively hydrogen bond donating and accepting sites in the receptor while L1, L2, and L3 denote lipophilic binding sites. |
The term benzodiazepine is the chemical name for the
Benzodiazepine drugs are substituted 1,4-benzodiazepines, although the chemical term can refer to many other compounds which do not have useful pharmacological properties. Different benzodiazepine drugs have different side groups attached to this central structure. The different side groups affect the binding of the molecule to the GABAA receptor and so modulate the pharmacological properties.[92] Many of the pharmacologically active “classical” benzodiazepine drugs contain the 5-phenyl-1H-benzo[e][1,4]diazepin-2(3H)-one substructure (see figure to the right).[97]
Nonbenzodiazepines also bind to the benzodiazepine binding site on the GABAA receptor and possess similar pharmacological properties. While the nonbenzodiazepines are by definition structurally unrelated to the benzodiazepines, both classes of drugs share a common pharmacophore (see figure to the lower right) which explains their binding to a common receptor site.[95]
[edit] Mechanism of action
Benzodiazepines work by increasing the efficiency of a natural brain chemical, GABA, to decrease the excitability of certain types of brain cells called neurons. This reduces the communication between neurons and therefore has a calming effect on many of the functions of the brain.

Schematic diagram of the (α1)2(β2)2(γ2) GABAA receptor complex which depicts the five protein subunits that form the receptor, the chloride (Cl–) ion channel pore at the center, the two GABA active binding sites at the α1 and β2 interfaces and the benzodiazepine (BZD) allosteric binding site at the α1 and γ2 interface.
GABA controls the excitability of neurons by binding to the GABAA receptor.[92] The GABAA receptor is a protein complex located in the synapses of neurons. All GABAA receptors contain an ion channel that conducts chloride ions across neuronal cell membranes and two binding sites for the neurotransmitter gamma-aminobutyric acid (GABA), while a subset of GABAA receptor complexes also contain a single binding site for benzodiazepines. Binding of benzodiazepines to this receptor complex promotes binding of GABA, which in turn increases the conduction of chloride ions across the neuronal cell membrane. This increased conductance raises the membrane potential of the neuron resulting in inhibition of neuronal firing. In addition, different GABAA receptor subtypes have varying distributions within different regions of the brain and therefore control distinct neuronal circuits. Hence, activation of different GABAA receptor subtypes by benzodiazepines may result in distinct pharmacological actions.[98] In terms of the mechanism of action of benzodiazepines, their similarities are too great to separate them into individual categories such as anxiolytic or hypnotic. For example, a hypnotic administered in low doses will produce anxiety relieving effects, whereas a benzodiazepine marketed as an anti-anxiety drug will at higher doses induce sleep.[99]
The subset of GABAA receptors that also bind benzodiazepines are referred to as benzodiazepine receptors (BzR). The GABAA receptor is a heteromer composed of five subunits, most commonly two α’s, two β’s and one γ (α2β2γ). For each subunit, many subtypes exist (α1-6, β1-3 and γ1-3). GABAA receptors that are made up of different combinations of subunit subtypes have different properties, different distributions in the brain and different activities relative to pharmacological and clinical effects.[100] Benzodiazepines bind at the interface of the α and γ subunits on the GABAA receptor. Binding also requires that alpha subunits contain a histidine amino acid residue, (i.e.,
Once bound to the benzodiazepine receptor, the benzodiazepine ligand locks the benzodiazepine receptor into a conformation in which it has a greater affinity for the
The benzodiazepine class of drugs also interact with peripheral benzodiazepine receptors.
[edit] Pharmacokinetics
A benzodiazepine can be placed into one of three groups by its
- Short-acting compounds have a half-life of 1–8 hours. They have few residual effects if taken before bedtime,
rebound insomnia may occur upon discontinuation and they might cause day time withdrawal symptoms such as next day rebound anxiety with prolonged usage. Examples are brotizolam, midazolam and triazolam.
- Intermediate-acting compounds have a half-life of 8–40 hours. They may have some residual effects in the first half of the day if used as a hypnotic. Rebound insomnia, however, is more common upon discontinuation of intermediate-acting benzodiazepines than longer acting benzodiazepines. Examples are estazolam, flunitrazepam, lormetazepam, nitrazepam and temazepam.
- Long-acting compounds have a half-life of 40–200 hours. They have a risk of accumulation in the elderly and in individuals with severely impaired liver function, but they have a reduced severity of
rebound effects and withdrawal. Examples are diazepam and chlordiazepoxide.
[edit] Interactions
Individual benzodiazepines may have different interactions with certain drugs. Depending on their metabolism pathway, benzodiazepines can be roughly divided into two groups. The largest group consists of those that are metabolized by cytochrome P450 (CYP450) enzymes and possess significant potential for interactions with other drugs. The other group comprises those that are metabolized through glucuronidation, such as lorazepam, oxazepam and temazepam and generally have few drug interactions.[77]
Many drugs, including oral contraceptives, some antibiotics, antidepressants and
[edit] Overdose
The use of Flumazenil is controversial following benzodiazepine overdose.
Although benzodiazepines are much safer in overdose than their predecessors, the barbiturates, they can still cause problems in overdose.[12] Taken alone, they rarely cause severe complications in overdose;[106] statistics in England showed that benzodiazepines were responsible for 3.8% of all deaths by poisoning from a single drug.[13] However, combining these drugs with alcohol,
A reversal agent for benzodiazepines exists, flumazenil (Anexate). Its use as an antidote in an overdose however is controversial.[111] Numerous contraindications to its use exist. It is contraindicated in patients with a history of long term use of benzodiazepines, those who have ingested a substance that lowers the seizure threshold or may cause an
[edit] Drug misuse

Alprazolam “Bars” 2 mg tablets
Benzodiazepines are considered major drugs of abuse.[15] Internationally, benzodiazepines are categorized as Schedule IV controlled drugs, apart from flunitrazepam which is a Schedule III drug under the Convention on Psychotropic Substances.[114] Some variation in drug scheduling exists in individual countries; for example in the United Kingdom midazolam and temazepam are Schedule III controlled drugs.[115] Benzodiazepine abuse ranges from occasional binges on large doses, to chronic and compulsive drug abuse of high doses.[116] Benzodiazepine abuse is mostly limited to individuals who abuse other drugs, i.e. poly-drug abusers. The majority of prescribed users do not abuse their medication.[117]
Benzodiazepines are used recreationally and by problematic drug misusers. Mortality is higher among poly-drug misusers that also use benzodiazepines. Heavy alcohol use also increases mortality among poly-drug users.[13] Dependence and tolerance, often coupled with dosage escalation, to benzodiazepines can develop rapidly among drug misusers; withdrawal syndrome may appear after as little as three weeks of continuous use. Long-term use has the potential to cause both physical and psychological dependence and severe withdrawal symptoms such as
A 1999–2005 Australian police survey of detainees reported preliminary findings that self-reported users of benzodiazepines were less likely than non-user detainees to work full-time and more likely to receive government benefits, use methamphetamine or heroin and be arrested or imprisoned.[119] Benzodiazepines are sometimes used for criminal purposes; they serve to incapacitate a victim in cases of
[edit] Veterinary use
Benzodiazepines are used in
[edit] References
- ^ a b Shorter E (2005). “Benzodiazepines”. A Historical Dictionary of Psychiatry. Oxford University Press. pp. 41–2. ISBN 0-19-517668-5.
- ^ a b Page C, Michael C, Sutter M, Walker M, Hoffman BB (2002). Integrated Pharmacology (2nd ed.). C.V. Mosby. ISBN 978-0723432210.
- ^ a b Olkkola KT, Ahonen J (2008). “Midazolam and other benzodiazepines”. Handb Exp Pharmacol 182 (182): 335–60. doi:10.1007/978-3-540-74806-9_16. PMID 18175099.
- ^ a b Dikeos DG, Theleritis CG, Soldatos CR (2008). “Benzodiazepines: effects on sleep”. in Pandi-Perumal SR, Verster JC, Monti JM, Lader M, Langer SZ (eds.). Sleep Disorders: Diagnosis and Therapeutics. Informa Healthcare. pp. 220–2. ISBN 0-415-43818-7.
- ^ a b Saïas T, Gallarda T (2008). “[Paradoxical aggressive reactions to benzodiazepine use: a review]” (in French). Encephale 34 (4): 330–6. doi:10.1016/j.encep.2007.05.005. PMID 18922233.
- ^ a b Lader M (2008). “Effectiveness of benzodiazepines: do they work or not?“. Expert Rev Neurother 8 (8): 1189–91. doi:10.1586/14737175.8.8.1189. PMID 18671662. http://www.expert-reviews.com/doi/full/10.1586/14737175.8.8.1189.
- ^ a b c d Lader M, Tylee A, Donoghue J (2009). “Withdrawing benzodiazepines in primary care”. CNS Drugs 23 (1): 19–34. doi:10.2165/0023210-200923010-00002. PMID 19062773.
- ^ a b c d e f g h i Ashton H (2005). “The diagnosis and management of benzodiazepine dependence” (PDF). Curr Opin Psychiatry 18 (3): 249–55. doi:10.1097/01.yco.0000165594.60434.84. PMID 16639148. http://www.benzo.org.uk/amisc/ashdiag.pdf.
- ^ a b c Ashton H (2004). “Benzodiazepine dependence”. in Haddad P, Dursun S, Deakin B (eds.). Adverse Syndromes and Psychiatric Drugs: A Clinical Guide. Oxford University Press. pp. 239–60. ISBN 978-0198527480.
- ^ a b c McIntosh A, Semple D, Smyth R, Burns J, Darjee R (2005). “Depressants”. Oxford Handbook of Psychiatry (1st ed.). Oxford University Press. p. 540. ISBN 0-19-852783-7.
- ^ a b c American College of Obstetricians and Gynecologists Committee on Practice Bulletins—Obstetrics (2008). “ACOG Practice Bulletin no. 92: Use of psychiatric medications during pregnancy and lactation” (PDF). Obstet Gynecol 111 (4): 1001–20. doi:10.1097/AOG.0b013e31816fd910 (inactive 2009-06-14). PMID 18378767. http://whb.ncpublichealth.com/provPart/docs/psychmeds.pdf
. Retrieved 2009-06-14. - ^ a b Fraser AD (1998). “Use and abuse of the benzodiazepines”. Ther Drug Monit 20 (5): 481–9. doi:10.1097/00007691-199810000-00007. PMID 9780123.
- ^ a b c Charlson F, Degenhardt L, McLaren J, Hall W, Lynskey M (2009). “A systematic review of research examining benzodiazepine-related mortality”. Pharmacoepidemiol Drug Saf 18 (2): 93–103. doi:10.1002/pds.1694. PMID 19125401.
- ^ a b White JM, Irvine RJ (1999). “Mechanisms of fatal opioid overdose”. Addiction 94 (7): 961–72. doi:10.1046/j.1360-0443.1999.9479612.x. PMID 10707430.
- ^ a b Lader MH (1999). “Limitations on the use of benzodiazepines in anxiety and insomnia: are they justified?”. Eur Neuropsychopharmacol 9 (Suppl 6): S399–405. doi:10.1016/S0924-977X(99)00051-6. PMID 10622686.
- ^ Sternbach LH (1979). “The benzodiazepine story”. J Med Chem 22 (1): 1–7. doi:10.1021/jm00187a001. PMID 34039. “During this cleanup operation, my co-worker, Earl Reeder, drew my attention to a few hundred milligrams of two products, a nicely crystalline base and its hydrochloride. Both the base, which had been prepared by treating the quinazoline N-oxide 11 with methylamine, and its hydrochloride had been made sometime in 1955. The products were not submitted for pharmacological testing at that time because of our involvement with other problems”.
- ^ Miller NS, Gold MS (1990). “Benzodiazepines: reconsidered”. Adv Alcohol Subst Abuse 8 (3–4): 67–84. PMID 1971487.
- ^ King MB (1992). “Is there still a role for benzodiazepines in general practice?” (PDF). Br J Gen Pract 42 (358): 202–5. PMID 1389432. PMC: 1372025. http://www.pubmedcentral.nih.gov/picrender.fcgi?artid=1372025&blobtype=pdf.
- ^ Peart R (1999-06-01). “Memorandum by Dr Reg Peart“. Minutes of Evidence. Select Committee on Health, House of Commons, UK Parliament. http://www.publications.parliament.uk/pa/cm199899/cmselect/cmhealth/549/99072723.htm
. Retrieved 2009-05-27. - ^ Tariq SH, Pulisetty S (2008). “Pharmacotherapy for insomnia”. Clin Geriatr Med 24 (1): 93–105, vii. doi:10.1016/j.cger.2007.08.009. PMID 18035234.
- ^ Lemmer B (2007). “The sleep–wake cycle and sleeping pills”. Physiol Behav 90 (2–3): 285–93. doi:10.1016/j.physbeh.2006.09.006. PMID 17049955.
- ^ a b c d e f g h Royal Pharmaceutical Society of Great Britain (2009). British National Formulary (BNF 57). BMJ Group and RPS Publishing. ISBN 9780853698456.
- ^ a b Perugi G, Frare F, Toni C (2007). “Diagnosis and treatment of agoraphobia with panic disorder”. CNS Drugs 21 (9): 741–64. doi:10.2165/00023210-200721090-00004. PMID 17696574.
- ^ Tesar GE (1990). “High-potency benzodiazepines for short-term management of panic disorder: the U.S. experience”. J Clin Psychiatry 51 (Suppl): 4–10; discussion 50–3. PMID 1970816.
- ^ Faught E (2004). “Treatment of refractory primary generalized epilepsy”. Rev Neurol Dis 1 (Suppl 1): S34–43. PMID 16400293.
- ^ Allgulander C, Bandelow B, Hollander E et al. (2003). “WCA recommendations for the long-term treatment of generalized anxiety disorder”. CNS Spectr 8 (Suppl 1): 53–61. PMID 14767398.
- ^ Stevens JC, Pollack MH (2005). “Benzodiazepines in clinical practice: consideration of their long-term use and alternative agents”. Journal of Clinical Psychiatry 66 (Suppl 2): 21–27. PMID 15762816. “The frequent use of benzodiazepines for the treatment of anxiety is likely a reflection of their effectiveness, rapid onset of anxiolytic effect, and tolerability.”.
- ^ a b c d e f McIntosh A, Cohen A, Turnbull N et al. (2004). “Clinical guidelines and evidence review for panic disorder and generalised anxiety disorder” (PDF). National Collaborating Centre for Primary Care. http://www.nice.org.uk/nicemedia/pdf/cg022fullguideline.pdf
. Retrieved 2009-06-16. - ^ Bandelow B, Zohar J, Hollander E, Kasper S, Möller HJ (October 2002). “World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the pharmacological treatment of anxiety, obsessive-compulsive and posttraumatic stress disorders”. World J. Biol. Psychiatry 3 (4): 171–99. PMID 12516310.
- ^ a b c Work Group on Panic Disorder (January 2009). “APA Practice Guideline for the Treatment of Patients With Panic Disorder, Second Edition” (PDF). http://www.psychiatryonline.com/pracGuide/loadGuidelinePdf.aspx?file=PanicDisorder_2e_PracticeGuideline
. Retrieved 07/12/09. - ^ Barbui C, Cipriani A (2009). “Proposal for the inclusion in the WHO Model List of Essential Medicines of a selective serotonin-reuptake inhibitor for Generalised Anxiety Disorder” (PDF). WHO Collaborating Centre for Research and Training in Mental Health. http://who.int/selection_medicines/committees/expert/17/application/Section24_GAD.pdf
. Retrieved 2009-06-23. - ^ Cloos JM, Ferreira V (2009). “Current use of benzodiazepines in anxiety disorders”. Current Opinion in Psychiatry 22 (1): 90–95. doi:10.1097/YCO.0b013e32831a473d. PMID 19122540.
- ^ Martin JL, Sainz-Pardo M, Furukawa TA, Martín-Sánchez E, Seoane T, Galán C (September 2007). “Benzodiazepines in generalized anxiety disorder: heterogeneity of outcomes based on a systematic review and meta-analysis of clinical trials”. J. Psychopharmacol. (Oxford) 21 (7): 774–82. doi:10.1177/0269881107077355. PMID 17881433.
- ^ “Clinical Guideline 22 (amended). Anxiety: management of anxiety (panic disorder, with or without agoraphobia, and generalised anxiety disorder) in adults in primary, secondary and community care” (PDF). National Institute for Health and Clinical Excellence. 2007. p. 23-25. http://www.nice.org.uk/nicemedia/pdf/CG022NICEguidelineamended.pdf
. Retrieved 2009-08-08. - ^ Canadian Psychiatric Association (July 2006). “Clinical practice guidelines. Management of anxiety disorders” (PDF). Can J Psychiatry 51 (8 Suppl 2): 51S–55S. PMID 16933543. http://publications.cpa-apc.org/media.php?mid=440&xwm=true
. Retrieved 2009-08-08. - ^ a b c d “Technology Appraisal Guidance 77. Guidance on the use of zaleplon, zolpidem and zopiclone for the short-term management of insomnia” (PDF). National Institute for Clinical Excellence. April 2004. http://www.nice.org.uk/nicemedia/pdf/TA077fullguidance.pdf
. Retrieved 2009-07-26. - ^ a b c Ramakrishnan K, Scheid DC (August 2007). “Treatment options for insomnia“. Am Fam Physician 76 (4): 517–26. PMID 17853625. http://www.aafp.org/afp/20070815/517.html.
- ^ a b c Buscemi N, Vandermeer B, Friesen C, Bialy L, Tubman M, Ospina M, Klassen TP, Witmans M (June 2005). “Manifestations and Management of Chronic Insomnia in Adults. Agency for Healthcare Research and Quality. Evidence Report/Technology Assessment Number 125” (PDF). http://www.ahrq.gov/clinic/epcsums/insomnsum.htm.
- ^ “What’s wrong with prescribing hypnotics?”. Drug Ther Bull 42 (12): 89–93. 2004. doi:10.1136/dtb.2004.421289. PMID 15587763. NeLM summary.
- ^ Scottish Intercollegiate Guidelines Network (2005). “Diagnosis and management of epilepsy in adults” (PDF). pp. 17–19. http://sign.ac.uk/pdf/sign70.pdf
. Retrieved 2009-06-05. - ^ a b Stokes T, Shaw EJ, Juarez-Garcia A, Camosso-Stefinovic J, Baker R (2004). “Clinical Guidelines and Evidence Review for the Epilepsies: diagnosis and management in adults and children in primary and secondary care” (PDF). Royal College of General Practitioners. pp. 61, 64–65. http://www.nice.org.uk/nicemedia/pdf/CG020fullguideline.pdf
. Retrieved 2009-06-02. - ^ a b c Shorvon SD (2009). “Drug treatment of epilepsy in the century of the ILAE: the second 50 years, 1959–2009“. Epilepsia 50 (Suppl 3): 93–130. doi:10.1111/j.1528-1167.2009.02042.x. PMID 19298435. http://www3.interscience.wiley.com/cgi-bin/fulltext/122250225/HTMLSTART.
- ^ Stokes T, Shaw EJ, Juarez-Garcia A, Camosso-Stefinovic J, Baker R (2004). “Clinical Guidelines and Evidence Review for the Epilepsies: diagnosis and management in adults and children in primary and secondary care (Appendix B)” (PDF). Royal College of General Practitioners. p. 432. http://www.nice.org.uk/nicemedia/pdf/CG020fullguideline_appendixB.pdf
. Retrieved 2009-06-02. - ^ Ashworth M, Gerada C (1997). “ABC of mental health. Addiction and dependence–II: Alcohol” (PDF). BMJ 315 (7104): 358–60. PMID 9270461. PMC: 2127236. http://www.pubmedcentral.nih.gov/picrender.fcgi?artid=2127236&blobtype=pdf.
- ^ Kraemer KL, Conigliaro J, Saitz R (1999). “Managing alcohol withdrawal in the elderly”. Drugs Aging 14 (6): 409–25. doi:10.2165/00002512-199914060-00002. PMID 10408740.
- ^ Prater CD, Miller KE, Zylstra RG (1999). “Outpatient detoxification of the addicted or alcoholic patient“. Am Fam Physician 60 (4): 1175–83. PMID 10507746. http://www.aafp.org/afp/990915ap/1175.html.
- ^ Ebell MH (2006). “Benzodiazepines for alcohol withdrawal“. Am Fam Physician 73 (7): 1191. PMID 16623205. http://www.aafp.org/afp/20060401/cochrane.html#c2.
- ^ Peppers MP (1996). “Benzodiazepines for alcohol withdrawal in the elderly and in patients with liver disease”. Pharmacotherapy 16 (1): 49–57. PMID 8700792.
- ^ a b c Tidy C (16 October 2007). “Pre-medication“. Patient UK. http://www.patient.co.uk/showdoc/40001448/
. Retrieved 2009-05-03. - ^ Mañon-Espaillat R, Mandel S (1999). “Diagnostic algorithms for neuromuscular diseases”. Clin Podiatr Med Surg 16 (1): 67–79. PMID 9929772.
- ^ Wyatt JP, Illingworth RN, Robertson CE, Clancy MJ, Munro PT (2005). “Poisoning”. Oxford Handbook of Accident and Emergency Medicine (2nd ed.). Oxford University Press. pp. 173–208. ISBN 978-0198526230.
- ^ Zimbroff DL (2008). “Pharmacological control of acute agitation: focus on intramuscular preparations”. CNS Drugs 22 (3): 199–212. doi:10.2165/00023210-200822030-00002. PMID 18278976.
- ^ Curtin F, Schulz P (2004). “Clonazepam and lorazepam in acute mania: a Bayesian meta-analysis”. J Affect Disord 78 (3): 201–8. doi:10.1016/S0165-0327(02)00317-8. PMID 15013244.
- ^ Gillies D, Beck A, McCloud A, Rathbone J, Gillies D (2005). “Benzodiazepines alone or in combination with antipsychotic drugs for acute psychosis”. Cochrane Database Syst Rev (4): CD003079. doi:10.1002/14651858.CD003079.pub2. PMID 16235313.
- ^ a b c d e Ballenger JC (2000). “Benzodiazepine receptors agonists and antagonists”. in Sadock VA, Sadock BJ, Kaplan HI (eds.). Kaplan & Sadock’s Comprehensive Textbook of Psychiatry (7th ed.). Lippincott Williams & Wilkins. pp. 2317–23. ISBN 0-683-30128-4.
- ^ a b Tasman A, Lieberman JA (2006). Handbook of Psychiatric Drugs. Wiley. p. 151. ISBN 0-470-02821-1.
- ^ Rapoport MJ, Lanctôt KL, Streiner DL et al. (2009). “Benzodiazepine use and driving: a meta-analysis”. J Clin Psychiatry 70 (5): 663–73. doi:10.4088/JCP.08m04325. PMID 19389334.
- ^ Orriols L, Salmi LR, Philip P et al. (2009). “The impact of medicinal drugs on traffic safety: a systematic review of epidemiological studies”. Pharmacoepidemiol Drug Saf. doi:10.1002/pds.1763. PMID 19418468.
- ^ “Benzodiazepines – oral“. MedicineNet. 2005. http://www.medicinenet.com/benzodiazepines-oral/article.htm
. Retrieved 2008-04-10. - ^ a b Paton C (2002). “Benzodiazepines and disinhibition: a review“. Psychiatr Bull R Coll Psychiatr 26 (12): 460–2. doi:10.1192/pb.26.12.460. http://pb.rcpsych.org/cgi/content/full/26/12/460.
- ^ Bond AJ (1998). “Drug-induced behavioural disinhibition: incidence, mechanisms and therapeutic implications”. CNS Drugs 9 (1): 41–57. doi:10.2165/00023210-199809010-00005.
- ^ Drummer OH (2002). “Benzodiazepines—effects on human performance and behavior” (PDF). Forensic Sci Rev 14 (1–2): 1–14. http://www.ndaa.org/pdf/ntlc_benzodiazepines.pdf
. Retrieved 2009-05-27. - ^ a b Ashton H (2007). “Drug dependency: benzodiazepines”. in Ayers S, Baum A, McManus C, Newman S (eds.). Cambridge Handbook of Psychology, Health and Medicine (2nd ed.). Cambridge University Press. pp. 675–8. ISBN 978-0521879972.
- ^ a b Barker MJ, Greenwood KM, Jackson M, Crowe SF (2004). “Cognitive effects of long-term benzodiazepine use: a meta-analysis”. CNS Drugs 18 (1): 37–48. PMID 14731058.
- ^ a b c Stewart SA (2005). “The effects of benzodiazepines on cognition” (PDF). J Clin Psychiatry 66 (Suppl 2): 9–13. PMID 15762814. http://psychiatrist.com/supplenet/v66s02/v66s0202.pdf.
- ^ Hammersley D, Beeley L (1996). “The effects of medication on counselling”. in Palmer S, Dainow S, Milner P (eds.). Counselling: The BACP Counselling Reader. 1. Sage. pp. 211–4. ISBN 978-0803974777.
- ^ Longo LP, Johnson B (2000). “Addiction: part I. Benzodiazepines—side effects, abuse risk and alternatives“. Am Fam Physician 61 (7): 2121–8. PMID 10779253. http://www.aafp.org/afp/20000401/2121.html.
- ^ Nardi AE, Perna G (May 2006). “Clonazepam in the treatment of psychiatric disorders: an update“. Int Clin Psychopharmacol 21 (3): 131–42. doi:10.1097/01.yic.0000194379.65460.a6. PMID 16528135. http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0268-1315&volume=21&issue=3&spage=131.
- ^ Otto MW, Bruce SE, Deckersbach T (2005). “Benzodiazepine use, cognitive impairment, and cognitive-behavioral therapy for anxiety disorders: issues in the treatment of a patient in need” (PDF). J Clin Psychiatry 66 (Suppl 2): 34–8. PMID 15762818. http://psychiatrist.com/supplenet/v66s02/v66s0206.pdf.
- ^ a b c Chouinard G (2004). “Issues in the clinical use of benzodiazepines: potency, withdrawal, and rebound” (PDF). J Clin Psychiatry 65 (Suppl 5): 7–12. PMID 15078112. http://psychiatrist.com/supplenet/v65s05/v65s0502.pdf.
- ^ Harrison PC, Gelder MG, Cowen P (2006). “The misuse of alcohol and drugs”. Shorter Oxford Textbook of Psychiatry (5th ed.). Oxford University Press. pp. 461–2. ISBN 0-19-856667-0.
- ^ Longmore M, Scally P, Collier J (2003). “Chapter 4”. Oxford Handbook of Clinical Specialties (6th ed.). Oxford University Press. p. 366. ISBN 0-19-852518-4.
- ^ Ashton H (1991). “Protracted withdrawal syndromes from benzodiazepines“. J Subst Abuse Treat 8 (1–2): 19–28. doi:10.1016/0740-5472(91)90023-4. PMID 1675688. http://benzo.org.uk/ashpws.htm.
- ^ a b c d Ashton CH (2002). “Benzodiazepines: how they work & how to withdraw“. The Ashton Manual. benzo.org.uk. http://benzo.org.uk/manual/
. Retrieved 2009-05-27. - ^ Lal R, Gupta S, Rao R, Kattimani S (2007). “Emergency management of substance overdose and withdrawal” (PDF). Substance Use Disorder. World Health Organisation. p. 82. http://www.whoindia.org/LinkFiles/Mental_Health_&_substance_Abuse_Emergency_management_of_Substance_Overdose_and_Withdrawal-Manual_For_Nursing_Personnel.pdf
. Retrieved 2009-06-06. “Generally, a longer-acting benzodiazepine such as chlordiazepoxide or diazepam is used and the initial dose titrated downward” - ^ Ebadi, Manuchair (23 October 2007). “Alphabetical presentation of drugs“. Desk Reference for Clinical Pharmacology (2nd ed.). USA: CRC Press. p. 512. ISBN 978-1420047431. http://books.google.co.uk/books?id=ihxyHbnj3qYC.
- ^ a b c d Meyler L, Aronson JK, ed (2006). Meyler’s Side Effects of Drugs: the International Encyclopedia of Adverse Drug Reactions and Interactions (15th ed.). Elsevier. pp. 429–43. ISBN 0-444-50998-4.
- ^ Committee on Safety of Medicines (1988). “Benzodiazepines, dependence and withdrawal symptoms” (PDF). Medicines and Healthcare products Regulatory Agency. http://www.mhra.gov.uk/home/idcplg?IdcService=GET_FILE&dDocName=CON2024428&RevisionSelectionMethod=LatestReleased
. Retrieved 2009-05-28. - ^ a b c d Moody D (2004). “Drug interactions with benzodiazepines”. in Raymon LP, Mozayani A (eds.). Handbook of Drug Interactions: a Clinical and Forensic Guide. Humana. pp. 3–88. ISBN 1-58829-211-8.
- ^ Roach SS, Ford SM (2006). “Sedatives and hypnotics”. Introductory Clinical Pharmacology (8th ed.). Lippincott Williams & Wilkins. p. 236. ISBN 978-0-7817-7595-3.
- ^ Dolovich LR, Addis A, Vaillancourt JM, Power JD, Koren G, Einarson TR (1998). “Benzodiazepine use in pregnancy and major malformations or oral cleft: meta-analysis of cohort and case-control studies“. BMJ 317 (7162): 839–43. PMID 9748174. PMC: 31092. http://www.bmj.com/cgi/content/full/317/7162/839.
- ^ American Academy of Pediatrics Committee on Drugs (1998). “Neonatal drug withdrawal“. Pediatrics 101 (6): 1079–88. PMID 9614425. http://pediatrics.aappublications.org/cgi/content/full/101/6/1079.
- ^ Iqbal MM, Sobhan T, Ryals T (2002). “Effects of commonly used benzodiazepines on the fetus, the neonate and the nursing infant“. Psychiatr Serv 53 (1): 39–49. doi:10.1176/appi.ps.53.1.39. PMID 11773648. http://ps.psychiatryonline.org/cgi/content/full/53/1/39.
- ^ a b Bogunovic OJ, Greenfield SF (2004). “Practical geriatrics: Use of benzodiazepines among elderly patients“. Psychiatr Serv 55 (3): 233–5. doi:10.1176/appi.ps.55.3.233. PMID 15001721. http://psychservices.psychiatryonline.org/cgi/content/full/55/3/233.
- ^ Bain KT (2006). “Management of chronic insomnia in elderly persons”. Am J Geriatr Pharmacother 4 (2): 168–92. doi:10.1016/j.amjopharm.2006.06.006. PMID 16860264.
- ^ Allain H, Bentué-Ferrer D, Polard E, Akwa Y, Patat A (2005). “Postural instability and consequent falls and hip fractures associated with use of hypnotics in the elderly: a comparative review”. Drugs Aging 22 (9): 749–65. doi:10.2165/00002512-200522090-00004. PMID 16156679.
- ^ Hulse GK, Lautenschlager NT, Tait RJ, Almeida OP (2005). “Dementia associated with alcohol and other drug use”. Int Psychogeriatr 17 (Suppl 1): S109–27. doi:10.1017/S1041610205001985. PMID 16240487.
- ^ Verdoux H, Lagnaoui R, Begaud B (2005). “Is benzodiazepine use a risk factor for cognitive decline and dementia? A literature review of epidemiological studies”. Psychol Med 35 (3): 307–15. doi:10.1017/S0033291704003897. PMID 15841867.
- ^ Snowden M, Sato K, Roy-Byrne P (2003). “Assessment and treatment of nursing home residents with depression or behavioral symptoms associated with dementia: a review of the literature”. J Am Geriatr Soc 51 (9): 1305–17. doi:10.1046/j.1532-5415.2003.51417.x. PMID 12919245.
- ^ Wang PS, Brookhart MA, Setoguchi S, Patrick AR, Schneeweiss S (2006). “Psychotropic medication use for behavioral symptoms of dementia”. Curr Neurol Neurosci Rep 6 (6): 490–5. doi:10.1007/s11910-006-0051-6. PMID 17074284.
- ^ Longo LP, Johnson B (April 2000). “Addiction: Part I. Benzodiazepines–side effects, abuse risk and alternatives“. Am Fam Physician 61 (7): 2121–8. PMID 10779253. http://www.aafp.org/afp/20000401/2121.html.
- ^ a b c Olsen RW, Betz H (2006). “GABA and glycine”. in Siegel GJ, Albers RW, Brady S, Price DD (eds.). Basic Neurochemistry: Molecular, Cellular and Medical Aspects (7th ed.). Elsevier. pp. 291–302. ISBN 0-12-088397-X.
- ^ a b Zavala F (1997). “Benzodiazepines, anxiety and immunity”. Pharmacol Ther 75 (3): 199–216. doi:10.1016/S0163-7258(97)00055-7. PMID 9504140.
- ^ a b Narimatsu E, Niiya T, Kawamata M, Namiki A (2006). “[The mechanisms of depression by benzodiazepines, barbiturates and propofol of excitatory synaptic transmissions mediated by adenosine neuromodulation]” (in Japanese). Masui 55 (6): 684–91. PMID 16780077.
- ^ a b Madsen U, Bräuner-Osborne H, Greenwood JR, Johansen TN, Krogsgaard-Larsen P, Liljefors T, Nielsen M, Frølund B (2005). “GABA and Glutamate receptor ligands and their therapeutic potential in CNS disorders”. in Gad SC. Drug Discovery Handbook. Hoboken, N.J: Wiley-Interscience/J. Wiley. pp. 797-907. ISBN 0-471-21384-5.
- ^ a b International Union of Pure and Applied Chemistry (1993). A Guide to IUPAC Nomenclature of Organic Compounds. Oxford: Blackwell Science. ISBN 0-632-03488-2. pp. 40–3.; Moss GP (1998). “Nomenclature of fused and bridged fused ring systems (IUPAC Recommendations 1998)” (PDF). Pure Appl Chem 70 (1): 143–216. doi:10.1351/pac199870010143. http://media.iupac.org/publications/pac/1998/pdf/7001×0143.pdf.
- ^ CAS registry number:2898-08-0 1,3-dihydro-5-phenyl-2H-1,4-benzodiazepin-2-one; other names: Ro 05-2921, dechlorodemethyldiazepam.
- ^ Rudolph U, Möhler H (2006). “GABA-based therapeutic approaches: GABAA receptor subtype functions”. Curr Opin Pharmacol 6 (1): 18–23. doi:10.1016/j.coph.2005.10.003. PMID 16376150.
- ^ Puri, Basant K.; Tyrer, Peter (28 August 1998). “Clinical psychopharmacology“. Sciences Basic to Psychiatry (2nd ed.). Churchill Livingstone. pp. 155-156. ISBN 978-0443055140. http://books.google.co.uk/books?id=KTbfRIqjLtUC&pg=PA149
. Retrieved 11-07-2009. - ^ Johnston GA (1996). “GABAA receptor pharmacology”. Pharmacol Ther 69 (3): 173–98. doi:10.1016/0163-7258(95)02043-8. PMID 8783370.
- ^ Wafford KA, Macaulay AJ, Fradley R, O’Meara GF, Reynolds DS, Rosahl TW (2004). “Differentiating the role of gamma-aminobutyric acid type A (GABAA) receptor subtypes”. Biochem Soc Trans 32 (Pt3): 553–6. doi:10.1042/BST0320553. PMID 15157182.
- ^ Hevers W, Lüddens H (1998). “The diversity of GABAA receptors. Pharmacological and electrophysiological properties of GABAA channel subtypes”. Mol Neurobiol 18 (1): 35–86. doi:10.1007/BF02741459. PMID 9824848.
- ^ Arvat E, Giordano R, Grottoli S, Ghigo E (2002). “Benzodiazepines and anterior pituitary function”. J Endocrinol Invest 25 (8): 735–47. PMID 12240908.
- ^ Zisterer DM, Williams DC (1997). “Peripheral-type benzodiazepine receptors”. Gen Pharmacol 29 (3): 305–14. doi:10.1016/S0306-3623(96)00473-9. PMID 9378234.
- ^ a b Norman TR, Ellen SR, Burrows GD (1997). “Benzodiazepines in anxiety disorders: managing therapeutics and dependence” (PDF). Med J Aust 167 (9): 490–5. PMID 9397065. http://www.mja.com.au/public/mentalhealth/course/06norman.pdf.
- ^ Gaudreault P, Guay J, Thivierge RL, Verdy I (1991). “Benzodiazepine poisoning. Clinical and pharmacological considerations and treatment”. Drug Saf 6 (4): 247–65. doi:10.2165/00002018-199106040-00003. PMID 1888441.
- ^ Green RS, Godsoe SK, Sharma S, Palatnick W (2008). “Toxicity, benzodiazepine“. eMedicine. http://emedicine.medscape.com/article/165645-print
. Retrieved 2008-06-10. - ^ a b Ramrakha P, Moore K (2004). “Chapter 14: Drug overdoses”. Oxford Handbook of Acute Medicine (2nd ed.). Oxford University Press. p. 791–838 (798). ISBN 0198520727.
- ^ Klein-Schwartz W, Oderda GM (1991). “Poisoning in the elderly. Epidemiological, clinical and management considerations”. Drugs Aging 1 (1): 67–89. doi:10.2165/00002512-199101010-00008. PMID 1794007.
- ^ Ramadan MI, Werder SF, Preskorn SH (2006). “Protect against drug–drug interactions with anxiolytics“. Curr Psychiatr 5 (5): 16–28. http://www.jfponline.com/Pages.asp?AID=4065.
- ^ Seger DL (2004). “Flumazenil—treatment or toxin”. J Toxicol Clin Toxicol 42 (2): 209–16. doi:10.1081/CLT-120030946. PMID 15214628.
- ^ Spivey WH (1992). “Flumazenil and seizures: analysis of 43 cases”. Clin Ther 14 (2): 292–305. PMID 1611650.
- ^ Goldfrank LR (2002). Goldfrank’s Toxicologic Emergencies. McGraw-Hill. ISBN 0-07-136001-8.
- ^ International Narcotics Control Board (2003). “List of psychotropic substances under international control” (PDF). http://www.incb.org/pdf/e/list/green.pdf
. Retrieved 2008-12-17. - ^ “List of drugs currently controlled under the misuse of drugs legislation” (PDF). UK Government Home Office. 2009-01-28. http://www.homeoffice.gov.uk/documents/cdlist.pdf?view=Binary
. Retrieved 2009-05-27. - ^ Karch, Steven B. (20 December 2006). Drug Abuse Handbook (2nd ed.). United States of America: CRC Press. p. 217. ISBN 978-0849316906. http://books.google.co.uk/books?id=F0mUte90ATUC.
- ^ Caan, Woody; Belleroche, Jackie de, eds (11 April 2002). “Benzodiazepine abuse“. Drink, Drugs and Dependence: From Science to Clinical Practice (1st ed.). Routledge. pp. 197-211. ISBN 978-0415278911. http://books.google.co.uk/books?id=nPvbDUw4w5QC&pg=PA197.
- ^ Gerada C, Ashworth M (1997). “ABC of mental health. Addiction and dependence—I: Illicit drugs” (PDF). BMJ 315 (7103): 297–300. PMID 9274553. PMC: 2127199. http://www.pubmedcentral.nih.gov/picrender.fcgi?artid=2127199&blobtype=pdf.
- ^ Loxley W (2007). “Benzodiazepine use and harms among police detainees in Australia” (PDF). Trends Issues Crime Crim Justice (336). ISBN 978-1-921185-39-7. http://www.aic.gov.au/publications/tandi2/tandi336.pdf
. Retrieved 2009-06-10. - ^ Kintz P (2007). “Bioanalytical procedures for detection of chemical agents in hair in the case of drug-facilitated crimes”. Anal Bioanal Chem 388 (7): 1467–74. doi:10.1007/s00216-007-1209-z. PMID 17340077.
- ^ a b Kahn CM, Line S, Aiello SE, ed (2005). The Merck Veterinary Manual (9th ed.). Wiley. ISBN 0-911910-50-6. http://www.merckvetmanual.com/mvm/index.jsp
. Retrieved 2009-06-08. - ^ Frey HH (1989). “Anticonvulsant drugs used in the treatment of epilepsy”. Probl Vet Med 1 (4): 558–77. PMID 2520134.
- ^ Podell M (1996). “Seizures in dogs”. Vet Clin North Am Small Anim Pract 26 (4): 779–809. PMID 8813750.
- ^ Gross ME (2001). “Tranquilizers, α2-adrenergic agonists, and related agents”. in Adams RH (ed.). Veterinary Pharmacology and Therapeutics (8th ed.). Iowa State University Press. pp. 325–33. ISBN 0-8138-1743-9.
[edit] Further reading
- Ashton CH (2002). “Benzodiazepines: how they work & how to withdraw“. The Ashton Manual. benzo.org.uk. http://benzo.org.uk/manual/
. Retrieved 2009-06-09. - Ashton CH (2007). “Benzodiazepine equivalence table“. benzo.org.uk. http://benzo.org.uk/bzequiv.htm
. Retrieved 2009-06-09. - Fruchtengarten L (1998). “Benzodiazepines“. PIM G008. International Programme on Chemical Safety (IPCS) INCHEM. http://www.inchem.org/documents/pims/pharm/pimg008.htm
. Retrieved 2009-06-09. - Longo LP, Johnson B (2000). “Addiction: part I. Benzodiazepines—side effects, abuse risk and alternatives“. Am Fam Physician 61 (7): 2121–8. PMID 10779253. http://www.aafp.org/afp/20000401/2121.html.
- “The complete story of the benzodiazepines“. The Eaton T. Fores Research Center. 2005. http://www.etfrc.com/benzos1.htm
. Retrieved 2009-06-09. - “Benzodiazepines advanced consumer information“. Drugs.com. 2005-02-24. http://www.drugs.com/cons/benzodiazepines.html
. Retrieved 2009-06-09.
|
||


